The US healthcare system suffers from a serious condition: fragmentation. While serious, this issue isn’t terminal. Treating this problem will help remove many barriers to health, allowing more seniors to stay in their homes and reducing the burden on healthcare systems.
What Is Fragmented Care?
Fragmented care is when a disconnect between healthcare providers occurs. The risk of fragmentation in healthcare increases the more individual healthcare organizations operate within independent “silos.” These silos exist for many reasons, namely:
- Conflicts with funding
- Laws and guidelines
- Data management
- Specialization
Fragmented care has been an ongoing problem in the US in recent decades. However, since the COVID-19 pandemic, which accelerated the burden on an already strained system, it has become even more apparent that simply ignoring fragmentation is no longer sustainable.
Fragmented care is a source of many inequities in healthcare and negatively affects people and health systems alike. It is also an equal threat to both public and economic health. Therefore, policymakers and leaders must address this issue sooner rather than later.
Understanding Fragmented Care
What Causes Fragmented Care?
In a 2009 article, Dr. Kurt Strange wrote, “Knowledge advanced greatly in the modern era by making sense of complicated things by understanding their parts.” But over time, this led to specialization in every field, industry, and niche.
Naturally, specialization has prompted many incredible advancements. It has allowed experts in various fields to uncover novel ways of understanding complex systems and their synergistic natures.
But, Strange noted our understanding of the natural world and human behavior is fragmented. Consequently, much of the progress seen in biology, physics, and other fields due to specialization has not translated to healthcare.
Specialization allows us to acquire more information by devoting focus, energy, and resources to a single facet. However, the problem is that humans’ ability to integrate, prioritize, and personalize this technical information has not kept up this pace.
Strange states that this has hurt “our ability to turn information into knowledge and knowledge into wisdom.” In other words, we have all the information we need, but because we view it through such a focused window, we don’t know how to apply it to a problem.
Below are examples of pitfalls in the healthcare field that perpetuate care fragmentation.
Over-Specialization
The human body is an intricate, complex organism. While a doctor may be extraordinarily knowledgeable, it’s impossible to understand everything about the body well enough to diagnose specific problems. For this reason, the current medical model separates the body into components in which various physicians specialize.
This method isn’t a problem for people who only need treatment from one specialist. But it’s a different story for those with multiple conditions who require numerous specialists. Each professional focuses on their area of expertise, leaving patients to navigate multiple treatment paths that, while aligned, never directly cross. For this reason, the growing population of people with more than one chronic condition needs a more generalist process.
Lack Of Shared Responsibility
A lack of shared responsibility for individual patients’ overall health is an unintended consequence of specialization. As Strange explains, specialization may lead some healthcare professionals to asses an issue exclusively within their area of expertise. However, by doing so, they overlook the person as a whole. This risks losing additional context that could better advise the course of treatment.
When somebody seeks treatment for a single condition, it’s much easier to determine who is responsible for the patient’s overall care and to clarify roles in the care process. But for people dealing with multiple conditions (and, subsequently, health providers), these questions often go unanswered as providers (and the flow of information between them) often remain siloed. This lack of shared responsibility perpetuates fragmented care.
Poor Communication With Caregivers
Despite being an invaluable source of information about a patient, informal caregivers often go overlooked in healthcare discussions. Unfortunately, poor communication with caregivers drives fragmented care because it keeps caregivers in their own silo.
In many cases, this disregard is unintentional. For example, many family caregivers work during the day, preventing them from attending appointments or meetings with their loved one’s care team during regular business hours.
No Shared Database For Patient Records
The absence of an electronic database makes it even more difficult for providers to coordinate care. Without a shared record where clinicians can access patients’ health data, even from other organizations, fragmented care will persist.
Suppose different specialists could easily access medical records from other specialists. In that case, they could get a more nuanced understanding of their patient’s specific health concerns. The creation of this type of system is perhaps the most direct and tangible way to solve fragmentation in healthcare.
Inadequate Time & Resources For Physicians
The human factor in healthcare is another driver behind fragmentation. Healthcare professionals are overwhelmed by labor shortages, high patient volume, and other problems. These problems were prevalent before the pandemic, but now, they are even worse.
Realistically, there is only so much that doctors can do to help their patients. After all, they are humans with physical limitations who face stringent demands on their bodies, minds, and resources.
In some cases, a specialist treating one of several conditions for a patient may lack the bandwidth to give a sufficient referral to another specialist, thus mitigating the chance of fragmentation.
Furthermore, even if doctors had the resources to do so, they often don’t receive reimbursement for their time or effort. Physicians should be compensated fairly for their work, just like any worker. Health system administrators could resolve this issue by giving physicians sufficient resources to make these referrals.
Effects Of Fragmented Care
Fragmentation is a latent issue, and its anonymous nature can inadvertently result in worse outcomes despite well-meaning efforts. It can also exasperate unmet needs, increase costs, and result in more hospital visits. Below are a few examples of the effects of fragmented care.
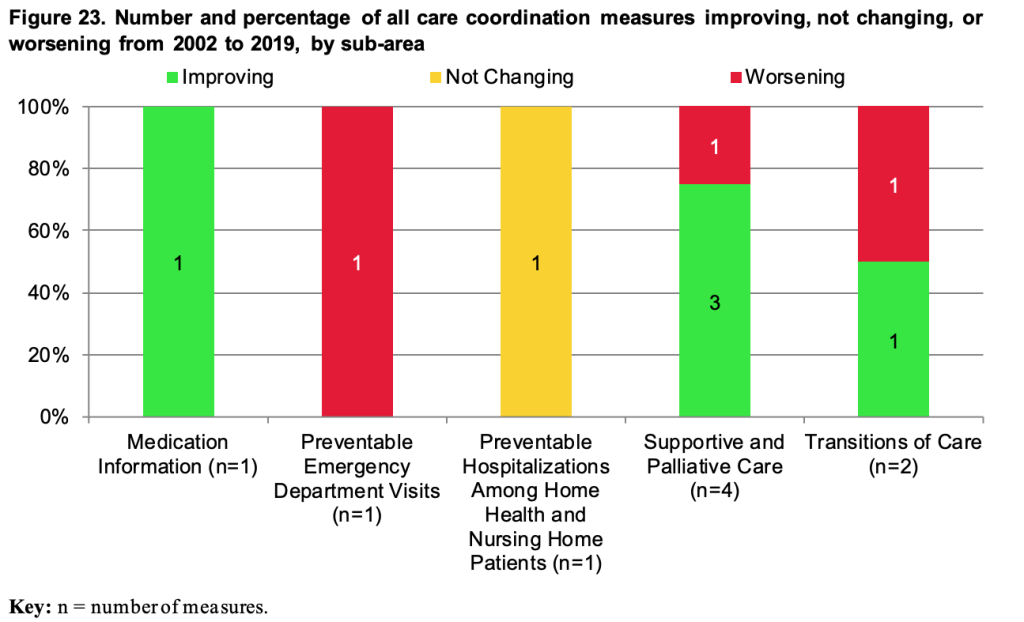
Increased Hospitalizations
Increased hospitalizations are among the most common consequences of a fragmented care system and primarily affect individuals with multiple long-term conditions.
According to a 2018 Commonwealth Fund study, Medicare recipients “with three to four chronic conditions and highly fragmented care were 14% more likely to visit the emergency department, and 6% more likely to have a hospital admission.”
Even patients with fewer health issues experienced higher rates of hospital visits because of fragmentation. For example, the Commonwealth Fund report found that people with just one health condition had a 13% higher likelihood of emergency department visits and a 14% higher risk of hospitalization.
Lower-Quality Care
The US spends more on healthcare than any country in the world. Yet, it consistently ranks among the lowest for quality. Growing research on fragmentation highlight this problem, citing fragmented care as one contributor to the country’s ineffective health system.
For example, Peterson-KFF Health System Tracker data shows,”Health spending per person in the US was $11,945 in 2020.” This rate was “over $4,000 more expensive than any other high-income nation.” Yet, despite these costs, many people feel that healthcare quality is lower than ever.
Despite this spending, the country’s health system lags far behind other developed nations. In a 2021 Commonwealth Fund report, researchers found that the US ranked last in all categories except “Care Process”:
- Access to Care
- Administrative Efficiency
- Equity
- Health Care Outcomes
Despite a slew of programs and services, the US healthcare system remains inefficient in delivering quality care. The current system is ideal for boosting profits for providers of goods and services in healthcare but dramatically contributes to inadequate healthcare delivery. An efficient healthcare system needs personalization and prioritization based on individual patients and their communities.
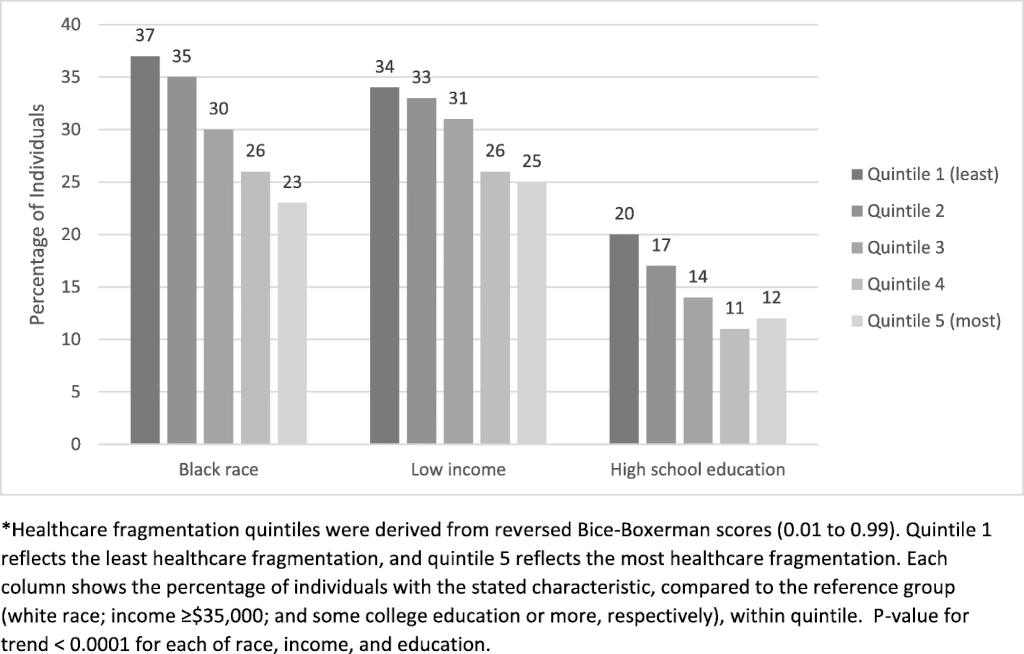
Inequality
“In a fragmented system, it is easy to ignore the poor,” Strange noted. He explains that when clinicians treat anyone who enters their office, they often don’t account for the numerous barriers they may have overcome to get there.
Another example is drug manufacturers who produce medications based on economic gain rather than for the common good. Or, the rise in for-profit hospitals and healthcare organizations can exclude many people seeking care.
Strange warns that it is easy for the most vulnerable to fall through the gaps in a fragmented system, even with social safety supports. Additionally, the ever-rising cost of healthcare worsens inequality by directing resources away from programs aimed at addressing social determinants of health that perpetuate this cycle.
Care Coordination: The Cure For Fragmented Care?
A firm grasp of the fundamental issue of fragmented care is a crucial baseline. That means looking at healthcare as an ever-changing aggregate rather than separate specialty areas.
This perception change is already underway, as many experts recognize the factors perpetuating fragmented care, such as specialization and outdated or restricted access to electronic records. But removing silos between health providers will require a substantial effort to implement and standardize care coordination.
What Is Care Coordination?
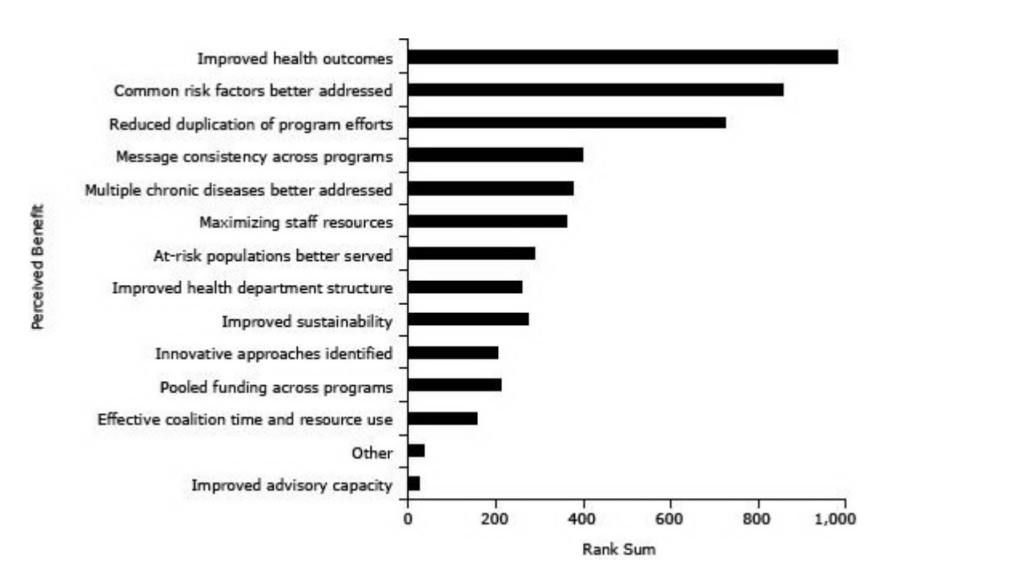
Care coordination refers to “deliberately organizing patient care activities and sharing information among all of the participants concerned with a patient’s care to achieve safer and more effective care.”
Care coordination aims to improve health outcomes and lower costs by avoiding preventable hospitalizations or unneeded tests or treatments. This is achieved by ensuring that health providers understand patients’ needs and priorities beforehand. It also provides this information is shared promptly with the right people involved in the care process and is used to deliver “safe, appropriate, and effective care.”
Many factors perpetuate fragmented care, namely, outdated or restricted access to electronic records and specialized health providers that operate independently within their own silos. However, health systems can streamline communication by implementing and refining care coordination methods.
MeetCaregivers Supports Efforts To End Fragmented Care
Most older adults want to age in place, but fragmented care can severely impact their ability to do so. Treating this problem like a public health issue will remove many barriers to health, allowing more seniors to stay in their homes and reducing the burden on healthcare systems.
Caregivers are critical to the solution because they offer a holistic view of each care recipient. In addition, they provide critical feedback about the home to any health professional; this often-overlooked perspective is crucial in assessing care needs and identifying barriers.
Marketplaces and platforms like MeetCaregivers improve financial accessibility by offering caregiving services as needed. Likewise, our solutions promote cohesive care:
- Seniors, families, care teams, and insurers can effectively communicate and share data through our Care Portal.
- We partner with Medicare Advantage plans to remove more friction points between seniors and home care services.
- Our Care Match program makes it easier to minimize gaps in care by seamlessness matching seniors and caregivers in a timely manner.
To learn how we can specifically help you, call 1 (888) 541-1136 or email info@meetcaregivers.com to chat directly with a care coordinator.
For more resources and information about fragmented care and social determinants of health, visit our Blog.
- Agha, L., Frandsen, B., & Rebitzer, J. B. (2019). Fragmented division of labor and healthcare costs: Evidence from moves across regions. Journal of Public Economics, 169, 144–159. https://doi.org/10.1016/j.jpubeco.2018.11.001
- Bynum, J. P., & Ross, J. S. (2013). A measure of care coordination?. Journal of general internal medicine, 28(3), 336–338. https://doi.org/10.1007/s11606-012-2269-0
- Diaz, S. (2018, February 15). The Implications of Fragmentation in Care. The Implications of Fragmentation in Care – Healthify. Retrieved September 19, 2022, from https://www.healthify.us/healthify-insights/the-implications-of-fragmentation-in-care
- Frandsen, B. R., Joynt, K. E., Rebitzer, J. B., & Jha, A. K. (2015). Care fragmentation, quality, and costs among chronically ill patients. The American journal of managed care, 21(5), 355–362
- Kaltenborn, Z., Paul, K., Kirsch, J. et al. Super fragmented: a nationally representative cross-sectional study exploring the fragmentation of inpatient care among super-utilizers. BMC Health Serv Res 21, 338 (2021). https://doi.org/10.1186/s12913-021-06323-5
- Kern, L. M. (2018, October 9). Whether Fragmented Care Is Hazardous Depends on How Many Chronic Conditions a Patient Has. Fragmented Care Chronic Conditions Overuse Hospital Services | Commonwealth Fund. Retrieved September 19, 2022, from https://www.commonwealthfund.org/publications/journal-article/2018/oct/fragmented-care-chronic-conditions-overuse-hospital
- Schneider, E. C., Shah, A., Doty, M. M., Tikkanen, R., Fields, K., & Williams II, R. D. (2021, August 4). Mirror, Mirror 2021: Reflecting Poorly. Mirror, Mirror 2021: Reflecting Poorly | Commonwealth Fund. Retrieved September 28, 2022, from https://www.commonwealthfund.org/publications/fund-reports/2021/aug/mirror-mirror-2021-reflecting-poorly
- Stange K. C. (2009). The problem of fragmentation and the need for integrative solutions. Annals of family medicine, 7(2), 100–103. https://doi.org/10.1370/afm.971
- Valentijn, P. (2021, July 30) Fragmentation of care: Its causes and what we can do about it. Retrieved September 19, 2022, from https://www.essenburgh.com/en/blog/fragmented-care-the-causes-and-what-we-can-do-about-it/
- Wager, E., Ortaliza, J., & Cox, C. (2022, January 21). How does health spending in the U.S. compare to other countries? How does health spending in the U.S. compare to other countries? – Peterson-KFF Health System Tracker. Retrieved September 28, 2022, from https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries-2/
